Causes and Treatment of Heel Spurs
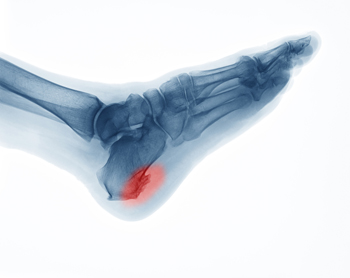
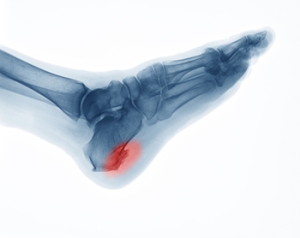
Heel spurs are bony protrusions that form on the bottom of the heel bone. They develop gradually from ongoing strain on the heel area, including repetitive stress activities like running or long periods of standing. The stress on the heel can lead to small tears in the tissues that attach to the heel, prompting the body to build extra bone as a defense mechanism. This becomes a heel spur. While not always painful, heel spurs can cause discomfort, especially when excessive pressure is placed on the heel. People with flat feet or high arches may be more prone to developing heel spurs. A podiatrist can diagnose heel spurs by conducting a physical examination and using imaging techniques like X-rays. Treatment usually involves non-surgical options, such as rest, wearing supportive footwear, or orthotic inserts designed to alleviate pressure on the heel. Surgery is only considered when symptoms persist despite these conservative treatments. If you believe you may have developed a heel spur, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our podiatrists from Ankle and Foot Centers of Missouri, P.C.. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our offices located in the Greater Kansas City area . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
Surgical Methods for Ingrown Toenails

Surgery for ingrown toenails is often necessary when conservative treatments fail to alleviate the pain and discomfort caused by the condition. Ingrown toenails occur when the edge of a toenail grows into the surrounding skin, typically affecting the big toe. This can lead to redness, swelling, severe pain and sometimes infection. A podiatrist can assess the severity of your ingrown toenail and may recommend a surgical procedure to remove part or all of the affected nail. In some cases, a portion of the nail’s matrix, or root, may also be removed to prevent regrowth. The procedure, which is usually done under local anesthesia, helps reduce the chances of recurrence. After surgery, patients are given guidelines for post-operative care to ensure proper healing and reduce the risk of infection. If you have developed a severely ingrown toenail, it is suggested that you promptly schedule an appointment with a podiatrist to see if nail removal is right for you.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact one of our podiatrists of Ankle and Foot Centers of Missouri, P.C.. Our doctors will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our offices located in the Greater Kansas City area . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot and Ankle Surgery
When conservative, noninvasive methods prove ineffective, surgery may be selected as the next course of action for the treatment of your foot or ankle condition. A wide number of foot and ankle surgical procedures exist, and it is up to your podiatrist to determine which intervention will be most appropriate and helpful for your case. Some surgical procedures include bunion surgery, fusion, hammertoe surgery, heel spur surgery, metatarsal surgery, nail surgery, neuroma surgery, reconstructive surgery, skin surgery, and tendon surgery. Typically, surgery is turned to as a definitive way to alleviate excessive pain or discomfort and to return your foot to full mobility.
Regardless of the location on the body, all surgical procedures require preoperative testing and examination to ensure the surgery’s success and preferred outcome. A review of your medical history and medical conditions will take place, as will an evaluation of any current diseases, illnesses, allergies, and medications. Tests such as blood studies, urinalyses, EKG, X-rays, and blood flow studies may be ordered. Because the procedure involves the foot and/or ankle, the structures of your feet while walking may also be observed by your podiatrist.
Care post-surgery will depend on the type of surgical procedure performed. Typically, all postoperative care involves rest, ice, compression, and elevation. To improve and ensure a safe recovery, your foot and ankle surgeon may also employ the use of bandages, splints, surgical shoes, casts, crutches, or canes. He will also determine if and when you can bear weight. A timely and thorough recovery is a priority for both you and your podiatrist, and carefully following postoperative instructions can help achieve this.
What Is Tarsal Tunnel Syndrome?

Tarsal tunnel syndrome is a condition that occurs when the tibial nerve is compressed as it passes through a narrow space in the ankle. Symptoms often include numbness, tingling, and burning sensations in the foot and toes. Individuals may also experience sharp or shooting pain that radiates from the ankle to the toes, particularly during activities that involve prolonged standing or walking.The causes of tarsal tunnel syndrome can vary widely. Common factors include flat feet, which can increase pressure on the nerve, as well as injuries or trauma to the ankle that result in swelling. Conditions such as diabetes, arthritis, or cysts may also contribute to nerve compression. If you have pain on the inside of the ankle, it is suggested that you consult a podiatrist who can provide an accurate diagnosis and treatment.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact one of our podiatrists of Ankle and Foot Centers of Missouri, P.C.. Our doctors can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our offices located in the Greater Kansas City area . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Treating Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which the tibial nerve, located in the tarsal tunnel in the foot, is compressed. The tibial nerve can become compressed from injury, such as an ankle sprain, flat feet, and lesions. Arthritis, diabetes, and varicose veins can also cause swelling and thus result in nerve compression.
Symptoms of tarsal tunnel syndrome include several different sensations in the sole of the foot, inside the ankle, and around the tibial nerve. These sensations include shooting pains, numbness or reduced sensation, pins and needles, burning, and tingling. Symptoms tend to worsen with greater activity to the area. In rare and severe occasions, this can change the muscles in the foot.
If you suspect you have tarsal tunnel syndrome, you should consult with your podiatrist. He or she will examine your medical history to see if you have a history of diabetes, arthritis, or flat feet. They will also check to see if you have suffered an injury to the area recently. An electrical test will be conducted to check if the nerve has been damaged. A simpler Tinel’s Test might also be used. This includes simply tapping the nerve to create a sensation. An MRI scan of the area may also be used.
Treatments vary greatly for tarsal tunnel syndrome. Treatments include both nonsurgical and surgical options depending upon the severity of the condition. Nonsurgical options include anti-inflammatory medication and steroid injections to the area. Orthotics, such as a splint or brace that immobilizes the foot, is another noninvasive option. For those with flat feet, custom shoes can be made to offer better foot support. Surgical options include a tunnel tarsal release, in which an incision is made behind the ankle down to the arch of the foot. This releases the ligament and relieves pressure off the nerve. Some doctors use a more minimally invasive surgery, where smaller incisions are made in the ankle and the ligament is stretched out.
If you are suffering from painful sensations in your foot, see a podiatrist who can determine if you are experiencing tarsal tunnel syndrome. Tarsal tunnel syndrome that is left unchecked can cause permanent nerve damage to the foot.
Facts About Heel Stress Fractures

A calcaneal stress fracture is a less common but painful source of heel pain. It often affects people who have recently increased their physical activity, such as starting a new exercise routine or hiking long distances. This type of stress fracture involves microscopic cracks in the heel bone that develop due to repetitive pounding. The pain usually appears gradually, creating a deep, aching sensation, rather than the sharp pain associated with conditions like plantar fasciitis. The pain may worsen with activity, making it difficult to walk without limping. Diagnosing calcaneal stress fractures can be challenging as initial X-rays may not detect the tiny cracks. Advanced imaging, such as MRI scans may be needed. Treatment involves immobilization and restricted weight-bearing for six to eight weeks, often requiring a special boot. If you have heel pain that may have resulted from a stress fracture, it is suggested that you schedule an appointment with a podiatrist.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact one of our podiatrists from Ankle and Foot Centers of Missouri, P.C.. Our doctors can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our offices located in the Greater Kansas City area . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.
See Your Foot Specialist Regularly If You Work On Your Feet
Achilles Tendonitis Recovery Solutions

Recovering from Achilles tendonitis can be a gradual process that requires patience and attention to your body’s signals. Returning to physical activities like running too early can lead to re-injury. For that reason, it is essential to wait until pain and stiffness are completely gone before resuming your normal routines. Once you are pain-free, start back by reducing both the mileage and frequency of your runs. Incorporate cross-training exercises, such as cycling or swimming, to help maintain fitness without putting stress on the Achilles tendon. Gradually build up your activity level to avoid overloading the tendon. A podiatrist can offer guidance on safe recovery exercises and assess whether custom orthotics or specific footwear might prevent future Achilles tendonitis problems. Regular check-ins are advised, as this foot doctor can identify any lingering issues and provide strategies to support long-term recovery. If you have sustained an Achilles tendon injury, it is suggested that you promptly schedule an appointment with a podiatrist.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Ankle and Foot Centers of Missouri, P.C.. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our offices located in the Greater Kansas City area . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.